State of Mind PREMIUM
Full Original Article
Outcome of Time Limited Psychotherapy for ‘Bulimic Spectrum Disorders’ in Routine Clinical Practice
Button, E.J. & Webb, C.L.
Eating Disorders Service, Leicestershire Partnership NHS Trust
Address for Correspondence: Dr. Eric Button, Eating Disorders Service, Brandon Unit, Leicester General Hospital, Leicester LE5 4PW;
e-mail: [email protected];
Tel: 0116 225 6328;
fax: 0116 225 6228.
Abstract
Objectives: Our aim was to explore treatment outcome for non-specific time-limited psychotherapy for bulimic spectrum disorders in routine clinical practice. Design: In view of the focus on outcome in routine clinical practice, we used a naturalistic design.
Methods. A total of 53 patients were successfully followed up and independently assessed on average at six months after completing such therapy and assigned to an improved or non-improved group based on evidence of a change to a less severe diagnosis.
Results. According to our criteria 60.4% were classed as ‘improved’, 37.7% showed no significant change and 1.9% (one patient) was judged to be worse. Improvement was greater in those with a lower initial score on the global severity index of the SCL90.
Conclusions. We consider the problems of measuring outcome in such patients, as well as the implications of the results for the psychotherapeutic management of bulimic spectrum patients with significant psychiatric co morbidity.
Introduction
Recurrent binge-eating, associated with significant psychological distress, is a common clinical problem in both specialised eating disorders services and more generic psychological and psychiatric services. This behaviour is most associated with bulimia nervosa (BN), which is mainly characterised by recurrent binge eating episodes and purging to compensate for the food eaten. In many cases, however, such symptomatology may not meet strict diagnostic criteria for bulimia nervosa. For example, the DSM IV specifies a minimum average of two binge / purge episodes a week for at least three months (American Psychiatric Association, 1994), but those who present with similar behaviours (e.g. less frequent binge / purge episodes, binge eating in the absence of purging behaviours) are referred to as Eating Disorders Not Otherwise Specified (EDNOS) in DSM IV. EDNOS also includes the subgroup referred to as binge eating disorder (BED), in which recurrent binge-eating occurs in the absence of regular use of compensatory behaviour, such as vomiting or laxative abuse. This study is concerned with the psychotherapeutic treatment of the full range of such symptomatology, which for the purposes of the present study we will refer to as ‘bulimic spectrum disorders’, a term which encompasses BN, BED and other eating disorders where there is a clinical problem of binge-eating in the absence of very low body weight. Such treatment is typically offered on a time-limited basis of between 16-20 sessions.
Clinical practice in the treatment of such disorders tends to be guided by empirically supported treatments evaluated in randomised controlled trials (RCTs) (e.g. National Institute for Clinical Excellence, 2004). There is evidence from a review of the many trials of psychotherapy and drug treatments for these disorders over the last few decades that a form of cognitive-behavioural therapy (CBT-BN) successfully improves some, if not all symptoms of BN (Agras, Walsh, & Fairburn, 2000; Fairburn, Jones & Peveler, 1993; Wilson & Fairburn, 1998 for a detailed review). Interpersonal psychotherapy (IPT) also has a clear evidence base and accordingly, is also recommended as a treatment for bulimia nervosa (Fairburn, 2000, Wilfrey, Agras, Telch, Rossiter, Schneider, Cole, Sifford & Raeburn, 1993). Given the similarities between many EDNOS cases and cases of BN (Fairburn, Cooper, Bohn, O’Connor, Doll & Palmer, 2007) it is expected these treatments would also benefit patients with an EDNOS diagnosis. Indeed, NICE (2004) makes similar recommendations to the above for the treatment of BED and related atypical eating disorders.
RCTs provide valuable information on the relative efficacy of different forms of psychotherapy carried out under controlled conditions. In the delivery of therapy in routine clinical practice, however, there is evidence that therapists are more flexible in the provision of treatment, often tailoring therapy to individual needs, and being guided by their personal experience, expertise and supervision, rather than predominantly basing clinical decisions on empirical data (Von Ranson & Robinson, 2006, Thompson-Brenner & Westen, 2005b). Outside of research trials, therapists are more likely to be trained in and practise treatments that integrate theoretical frameworks than those prescribed in therapy manuals (Tuschen-Caffier, Pook & Frank, 2001; Westen, Novotony, & Thompson-Brenner, 2004). Moreover, the duration of therapy can be longer than what is prescribed in the fixed term therapies characteristic of RCTs (Morrison et al, 2003; Thompson-Brenner & Western, 2005a). These differences may be due to an increased likelihood, outside of research trials, of addressing co-morbidity (Roth & Fonagy, 1996) rather than focusing on a single disorder (Morrison et al, 2003; Thompson-Brenner & Westen, 2005b).
Accordingly, therapy in routine clinical practice may often be qualitatively different from that in randomised clinical trials (Tuschen-Caffier et al, 2001). Given these apparent differences, there is an argument for studying treatment outcomes from patient samples in routine clinical settings in order to complement findings from RCTs in the development of treatments. Morrison et al (2003) argue that treatment recommendations can be drawn from assessing correlations between what clinicians do in their everyday practice and treatment outcome. As there is likely to be variety in what is practised and its effectiveness, they argue it is important to consider studying patterns of co-variation between treatment provision and outcome to aid the development of effective treatments. Exploring treatment provision and outcome data from routine clinical practice may provide a way of addressing some of the potential omissions of the literature provided by empirically supported therapies which have focused almost exclusively on brief, largely ‘CBT therapies’ taking place in controlled trails (Thompson-Brenner & Westen, 2005 a; Westen, Novotony & Thompson-Brenner, 2004).
This study focused on the delivery of non-specific time limited outpatient psychotherapy for patients presenting with ‘bulimic spectrum disorders’ (as defined above) delivered in routine clinical practice in a specialised eating disorder service for adults within the National Health Service. There were two broad aims:
- To investigate treatment outcome in routine clinical practice.
- To examine whether any patient and treatment characteristics were predictive of outcome.
We hoped to use this information to indicate those patients for whom time limited psychotherapy (‘TLP’) may be appropriate, as well as identifying those patients who may need a different approach.
METHOD
Procedure
In accordance with routine clinical practice in the service, those patients with bulimic spectrum disorders assessed as suitable for a course of ‘time-limited psychotherapy’ (TLP) and who were motivated to try this form of intervention, were placed on a waiting list for allocation to a therapist. The mean duration of waiting time to be offered a start date for therapy was 19.2 weeks (S.D=8.8). It was explained to patients that TLP would normally consist of 16-20 sessions, usually commencing on a weekly basis. The form of psychotherapy utilised varied according to a combination of patient problems and therapeutic orientation of therapists. Broadly speaking this included cognitive-behavioural (CBT – e.g. Fairburn, Cooper & Shafran, 2003), interpersonal (IPT – Birchall, 1999), personal construct (PCT – Button, 1985) and more integrative psychotherapeutic approaches. It should be stressed that all therapy was conducted according to ‘usual clinical practice’ in the multi-disciplinary team and not constrained by the requirements of a research trial. All therapists were either experienced and qualified in their therapeutic modality or received appropriate supervision from such an individual.
At the end of the course of TLP, there was approximately a four-month period when the patient was not seen by the service. At the end of this period it was routine practice that they were invited to attend for a review appointment, usually with their original assessor, rather than their therapist. In circumstances where the assessor and therapist was the same person, the review was conducted by a third party with experience in assessing eating-disordered patients. We only attempted to review those patients who completed at least a half of the allocated number of sessions (>=8). Those patients who did not take up the formal offer of a start date for therapy or who dropped out at an early stage in therapy (<8 sessions) were not formally reviewed for this study. We did, however, carry out a comparison of those reviewed and those not reviewed in order to assess representativeness (see below).
Participants
Subjects were drawn from a consecutive series of patients who had presented to a specialised eating disorders service over a three-year period between January 2004 and January 2007. Their initial assessment had concluded that they were suitable for a course of time-limited psychotherapy and that they met criteria for either bulimia nervosa or eating disorder not otherwise specified (including binge eating disorder), with regular (at least weekly) ‘objective’ binge-eating being present for at least three months. Patients with a Body Mass Index (BMI) less than 18.0 and/or a recent history of anorexia nervosa were excluded.
During the period of the study, 138 patients were offered TLP for ‘bulimic spectrum disorders’ and thus eligible for the study. They were predominantly young females, although seven (5.1%) were male and eighteen (13.0%) were age 40 or over. 67.2% were diagnosed as BN and 32.8% as EDNOS. Only 21.7% had previously received some form of psychiatric/psychotherapeutic treatment specifically for their eating disorder. In all cases, binge-eating was a significant aspect of their eating disorder. Most patients used some form of compensatory behaviour, most commonly self-induced vomiting, which occurred at least weekly in 68.8% of patients. In addition to their eating-disordered behaviour, as a group they showed elevated scores on the SCL90 (Global Severity Index mean = 1.74, SD = 0.76 ) and the Rosenberg Self-Esteem Scale (RSE) (mean= 4.81, SD = 1.53), thus indicative of wider mental health problems, as one would expect in such a population.
Out of the overall cohort, 24 never started; 32 attended 1-7 sessions; 28 attended therapy but failed to attend review; 1 patient where details were lost. The remaining 53 patients were reviewed at least four months (mean 26.5 weeks, S.D. 14.4) after completing therapy and comprised our main study sample, as outlined below.
Main Study Sample
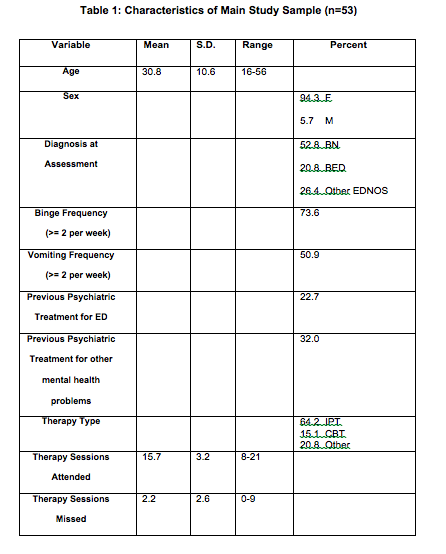
The characteristics of the main study sample are displayed in Table 1. We compared those reviewed (n=53) with those not reviewed (n=85) on a number of clinical and demographic variables. The only difference between groups was that those reviewed were older at initial presentation (t=2.838, d.f. 136, p<.001). In all other respects, there was no evidence that those followed up were in any way atypical of the cohort as a whole.
Measures and the Assessment of Outcome
As part of the Service’s routine assessment processes, all patients were asked to complete the following questionnaires at initial assessment and at review:
1. Eating Disorders Inventory (EDI) (original version) (Garner, Olmsted & Polivy, 1983)
2. Symptom Check List (SCL90) (Derogatis,1977)
3. Rosenberg Self-Esteem Scale (RSE) (Rosenberg, 1965)
In addition to such validated questionnaires, clinicians used an in-house standard rating scale of the frequency of key behaviours and concerns characteristic of eating disorders. This was based on the Clinical Eating Disorders Rating Instrument (‘CEDRI’) (Palmer, R.L., Christie, M., Cordle, C., Davies, D. & Kenrick, J., 1987), which is also incorporated into the service’s routine assessment.
Our main outcome criterion was based on the diagnosis at review compared with that at initial assessment. Diagnosis was according to DSMIV criteria and in each case this was based on a consensus judgement by the first two authors (EB and CW).
Improved
Where patients moved to what might be regarded as a less severe diagnosis and included:
- BN to EDNOS
- BN to No Eating Disorder
- EDNOS to No Eating Disorder
It should be noted that in our study this category would not apply in cases where there was any significant increase in frequency of either binge-eating or compensatory behaviour.
No Change
Where patients remained at the same diagnosis (i.e. BN or EDNOS)
Worse
Where patients moved to a more severe diagnosis (i.e. from EDNOS to BN)
Co-morbidity
We did initially consider making a comparison of co morbidity before therapy and at review, but robust data was not available on a sufficient number of patients to make this valid. We will, however, exemplify some of the issues around co-morbidity by means of case vignettes.
Statistical Analysis
All data was stored and analysed using SPSS version 16.0. Non-parametric statistical tests (Mann-Whitney and chi-square) were used to compare improvers with non-improvers.
RESULTS
Outcome
The breakdown of outcome was that 60.4% were categorised as ‘improved’, 37.7% ‘no change’ and 1.9% ‘worse’. At follow-up only 15.1% met criteria for bulimia nervosa and 37.7% were symptom-free from the eating disorder standpoint (i.e. no recent objective binge-eating or compensatory behaviour). The remainder (47.1%) were categorised as EDNOS.
Factors Associated with Outcome
In view of the fact that only one patient was categorised as worse, the improved group was compared to the non-improved group (comprising ‘no change’ and ‘worse’) on all variables. Two variables significantly differentiated between improvers and non-improvers. Lower score at initial assessment on the Global Severity Index of the SCL90 was found in improvers (Mann-Whitney U 148, p=.025). Moreover, those patients who received a form of CBT (n=8) were more likely to be improvers (chi-square 6.56, d.f. 2, p<.05). All eight patients who received CBT were improved, as opposed to 24/45(53.3%) of those receiving other forms of psychotherapy. In view of this finding, we compared those receiving CBT versus the remainder on pre-treatment variables and there was no evidence that they presented with less severe symptoms initially.
Problems in Measuring Outcome in this Study
In order to illustrate some of the difficulties of assessing outcome in bulimic spectrum disorders and to indicate how the use of different outcome measures is likely to result in different ‘improvement’ rates, two cases are briefly presented below:
Case Vignette: N
N was a 43 year old male, who presented with bulimia nervosa (purging type) and moderate depression over the past two years. He had had no previous treatment for his eating disorder, but he had attended general psychiatry out-patients a year or two ago for his depression. At initial presentation, he was bingeing 3-4 times a week, as well as vomiting and taking laxatives at similar frequency.
He received 17 sessions of IPT. When followed up five months after therapy, he was only bingeing occasionally (less than weekly), but his vomiting had increased to 2-3 times a day. His mood had improved. He was next followed up a further three months later, by which time he was eating regularly, not bingeing and vomiting had reduced to 1-2 times a week, his mood improvement having been sustained.
In this case, according to the binge-eating criterion, there is clear improvement at both 5 and 8 month follow-up, whereas in terms of vomiting there was deterioration, albeit followed by some improvement. Moreover, initial and sustained improvement in mood was not accompanied by marked improvement in eating behaviour.
In this study N, outcome was taken at the five month follow up point. N was rated ‘no significant change’, as despite having shifted from a diagnosis of BNP to EDNOS and reporting improved mood, his increase in vomiting indicated a severe level of eating disorder psychopathology remained.
Case Vignette: C
C was a 25 year old obese woman presenting with Binge Eating Disorder over the past four years. She had had no previous treatment for an eating disorder, but had received some counselling at general practice level for depression. At initial presentation, binge-eating was occurring five times a week, with no compensatory behaviour.
She received 16 sessions of IPT. At follow-up five months later, there had been only one binge-eating episode in the past five weeks, but questionnaire scores (EDI, SCL90, Rosenberg and Core) were unchanged and indicative of continuing moderate depressive symptoms and ongoing low self-esteem.
Thus, whilst improvement was identifiable in terms of the binge-eating criterion, there was considerable ongoing co-morbidity.
In this study outcome was rated as ‘significant improvement’. This was based on the change in eating disorder symptoms as this study did not include measures of co-morbidity to evaluate outcome.
DISCUSSION
The first aim of the study was to investigate treatment outcome for time-limited psychotherapy for ‘bulimic spectrum disorders’ in routine clinical practice. In this study outcome was examined by assessing ‘improvement’ in the group of patients who completed therapy and attended for a four month follow up review. Improvement was defined by movement from one eating disorder diagnosis to one that was considered less severe. Using this criterion, our results show that 60.4% of those who completed therapy had improved. However, not all of these were free of an eating disorder. In terms of diagnosis 37.7% had no eating disorder symptoms, 47.1% met criteria for EDNOS and 15.1% met criteria for BN.
This outcome appears to be comparable with those of other studies of time limited therapies for bulimic spectrum disorders, which report improvement rates as ranging from 39% – 70.1% (e.g. Agras et al, 2000; Fichter et al, 2008; Vrabel et al, 2008; Wilson and Fairburn, 1998).
This variation in ‘improvement’ in studies is due to a number of factors, the most common of which is the lack of agreement in defining and measuring outcome (Anderson & Maloney, 2001; Fassino, Piero, Levi, Gramaglia, Amianto, Leombruni, & Abbate Daga, 2004). Studies include a variety of diagnostic and outcome measures, reflecting numerous definitions of symptoms, remission, recovery and relapse; they rely on a variety of sources to assess outcome (i.e. patients, clinicians and independent / external assessors) and outcome may be reported at a variety of time periods post treatment. In this study we chose to measure a change from one eating disorder diagnostic category to a less severe category (as recorded in DSM-IV), as have other studies (e.g. Vrabel et al, 2008). However, as the case vignettes described above illustrate, defining outcome was not always straightforward. A shift from BN to the EDNOS category generally constituted a reduction in binge – purge behaviours. However this was not true in every case. For example Case Vignette ‘N’ significantly reduced binge-eating, but also increased purging behaviour significantly, resulting in a change of diagnosis from BNP to EDNOS, but an assessment outcome of ‘no significant change’. As explained above, even though a patient may have changed to a more favourable diagnosis, where there was any substantial increase in either binge-eating or compensatory behaviour we classified the outcome as ‘no change’. This is an important clinical point, and needs to be made explicit, when using a shift in diagnosis as a measure of outcome.
A second aim of this study was to examine whether any patient and treatment characteristics were predictive of outcome. This study identified two variables that appeared to predict improved outcome. The first was patient’s scores at initial assessment on the Global Severity Index (GSI) of the SCL-90, with lower scores on this measure, predicting superior treatment outcome. The GSI was taken as a crude measure of co morbidity and hence it appears that a higher level of co-morbidity as measured at initial assessment was a predictor of poorer treatment outcome. Other studies indicate the presence or indication of co-morbid problems as an indication of poor treatment outcome in the treatment of binge eating disorder and bulimia nervosa (e.g. Baell and Wertheim, 1992; Berkman, Lohr & Bulikl, 2007;Bossert, Schmolz, Wiegand, Junker & Kreig, 1992; Thompson-Brenner and Westen, 2005a). In some studies other predictors of global outcome have been identified, such as low self-esteem (Bell 2002), binge frequency and ‘ineffectiveness’ (Baell and Wertheim,1992), but the current study did not replicate these findings.
Complex patients presenting with pre treatment co-morbidity may need to be routinely offered additional or different treatment to the time limited therapies offered, which focus primarily on addressing the eating disorder. Westen and Hardern-Fischer (2001) comment that symptom focused treatments can help but may fail to address the personality structure that provides a context for understanding disordered eating patients. Indeed, given the increasing body of evidence showing that personality variables run alongside most mood, anxiety and eating disorders, they should be a focus of treatment alongside symptoms (Brown and Barlow, 1992; Westen et al, 2004; Thompson-Brenner & Westen, 2005a), to create a treatment approach more valid than current manualised treatments focusing solely on a specific set of symptoms.
Lengthening treatment may address this need as specific aspects of the co morbidity (e.g. depression, anxiety, personality issues, low self esteem, ‘ineffectiveness’) could then be addressed either by integrating specific symptom focused with co morbid / personality focused interventions from the beginning of therapy, or by addressing broader issues prior to addressing the eating disorder. An alternative way of addressing this issue is to develop a flexible (‘staged’) treatment approach whereby eating disorders symptoms are the initial focus of therapy but there is the flexibility to move to address broader psychopathology / issues if assessed as being clinically appropriate.
The second predictor of improvement indicated in this study is related to the type of time limited psychotherapy the patient received, with those who received CBT having improved outcome in comparison to those receiving other psychotherapeutic approaches. Analysis was conducted, which indicated that patients offered CBT at assessment were not ‘qualitatively different’ from those offered another type of therapy. This is an interesting finding, which appears to be consistent with current NICE Guidelines and research (Fassino et al, 2004, reviewed existing literature on psychological treatments for eating disorders and found evidence of the efficacy of CBT). However we would wish to be extremely cautious in drawing conclusions from this finding, given the very small numbers in the therapy subgroups.
The findings from the current study are limited by several factors. Firstly, this research is based on a single service over a three year period. Although it is likely that the patients presenting in this time are typical of those generally seen in this service, a larger cohort would have given more statistical power to the data.
Secondly, the main finding was restricted to patients who attended follow up appointments at four months post therapy. This was 53/81 patients (65.4%) of those who attended at least half of the allocated number of sessions, with approximately one third of those contacted failing to attend. Moreover, we did not have the resources to be able to attempt to assess those patients who dropped out at an early stage in treatment. This appears to reflect the difficulties in ‘real life’ service evaluation research of getting patients to attend appointments and/or complete questionnaires once their treatment has ended. The percentage of follow ups obtained in routine clinical practice is generally much smaller than among the participants of controlled trials (Tuschen-Caffier et al, 2001) and reflects the clinician’s general difficulties and resource constraints of ‘chasing’ patients who have been discharged from routine clinical practice. However it is a significant point with regard to evaluating outcome, as outcome levels have been shown to improve over time (e.g. Fitcher, Quadflieg & Gnutzmann, 1998; Fichter et al, 2008; Vrabel et al, 2008).
Thirdly, outcome in this study was limited to a primary analysis of eating disorder symptoms as we did not have consistent, detailed information on co-morbidity. Our measure of co morbidity came from the Global Severity Index of the SCL-90 and although this is a measure used in other studies to assess the presence of wider psychopathology, more specific tools such as the Beck Depression Inventory could have been administered. We would also have benefited from systematically collecting information regarding contact with general psychiatric services.
Finally, this study aimed to look at outcome in real life practice, thereby the therapists weren’t following manualised treatment packages. Accordingly we cannot make any claims about the relationship between specific interventions and outcome.
In conclusion, this small-scale service-evaluation study of time-limited psychotherapy in routine clinical practice found improvement rates broadly comparable to the range of outcomes deriving from current literature . However, as Fassino et al (2004) point out, the lack of consensus on how to define outcome in eating disorders is problematic and the use of different criteria of improvement could produce significantly different results. The predictors of ‘good outcome’ in this study were also consistent with the current research literature. We hope that our findings will stimulate further outcome research in routine clinical practice in other specialised eating disorder services, to complement findings from randomised clinical trials.
References
- Agras, W.S., Walsh, B.T., & Fairburn, C.G. (2000). A multi-centre comparison of cognitive behavioural therapy and interpersonal psychotherapy for bulimia nervosa. Archives of General Psychiatry, 57, 459-466.
- American Psychiatric Association (1994). Diagnostic and Statistical Manual fro Mental Disorders (4th edn.). Washington, D.C.: American Psychiatric Association.
- Anderson, D.A., & Maloney, K.C. (2001). The efficacy of cognitive behaviour therapy on the core symptoms of bulimia nervosa. Clinical Psychology Review. 21 (7), 971-988.
- Baell, W.K. & Wertheim, E.H. (1992). Predictors of outcome in the treatment of bulimia nervosa. British Journal of Clinical Psychology, 31, 330-332.
- Bell, L. (2002). Does concurrent psychopathology at presentation influence response to treatment for bulimia nervosa? Eating and Weight Disorders , 7, 168-81.
- Berkman, N.D., Lohr, K.N., & Bulik, C.M. (2007). Outcomes of eating disorders: a systematic review of the literature. International Journal of Eating Disorders, 40, 293-309.
- Birchall, H. (1999). Interpersonal psychotherapy in the treatment of eating disorders. European Eating Disorders Review, 7, 315-320.
- Bossert, S., Schmolz, U., Wiegand, M., Junker, M., & Kreig, J.C. (1992). Predictors of short term outcome in bulimia nervosa inpatients. Behaviour Research and Therapy, 30, 193-199.
- Brown, T.A., & Barlow, D.H. (1992). Co morbidity among the anxiety disorders: implications for treatment and the DSM-IV. Journal of Consulting and Clinical Psychology, 60, 835-844.
- Button, E.J. (1985). Eating Disorders: Personal Construct Therapy and Change. Chichester: Wiley.
- Derogatis, L.R. (1977) Administration, Scoring and Procedures for the SCL90R. Baltimore: Clinical Psychometric Research.
- Fairburn, C.G. (2000). Comparing IPT with CBT. Archives of General Psychiatry, 57, 459.
- Fairburn, C.G., Cooper, Z., Bohn, K., O’Connor, M.E., Doll, H.A., & Palmer R.L. (2007). The severity and status of eating disorder NOS. Implications for DSM-V. Behaviour Research and Therapy, 45, 1705 – 1715.
- Fairburn, C.G., Cooper, Z., & Shafran, R. (2003). Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behaviour Research and Therapy, 41, 509-528.
- Fairburn, C.G., Jones, R., & Peveler, R.C. (1993). Psychotherapy and bulimia nervosa: The longer term effects of interpersonal psychotherapy, behaviour therapy, behaviour therapy and cognitive behaviour therapy. Archives of General Psychiatry, 50, 419-428.
- Fassino, S., Piero, A., Levi, M., Gramaglia, C., Amianto, F., Leombruni, P., & Abbate Daga, G. (2004). Psychological treatment of eating disorders: A review of the literature. Panminerva Med., 46, 189-98.
- Fichter, M.M., Quadflieg, N., & Gnutzmann, A. (1998). Binge eating disorder: treatment outcome over a 6 year course. Journal of Psychosomatic Research, 44, 385-405.
- Fichter, M.M., Quadflieg, N., & Hedlund, S. (2008). Long-term course of binge eating disorder and bulimia nervosa: relevance for nosology and diagnostic criteria. International Journal of Eating Disorders (in press).
- Garner, D.M., Olmsted, M.P., & Polivy, J. (1983). Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders, 2, 15-34.
- Morrison, K.H., Bradley, R., & Westen, D. (2003). The external validity of controlled clinical trails of psychotherapy for depression and anxiety: A naturalistic study. Psychology and Psychotherapy: Theory, Research and Practice, 76, 109-132.
- National Institute for Clinical Excellence (2004). Eating Disorders: Core interventions in the treatment of anorexia nervosa, bulimia nervosa and related disorders. National Institute for Clinical Excellence.
- Palmer, R.L., Christie, C., Cordle, C., Davies, D., & Kenrick, J. (1987). The Clinical Eating Disorders Rating Instrument (CEDRI): a preliminary description. International Journal of Eating Disorders, 6, 9-16.
- Rosenberg, M. (1965). Society and the Adolescent Self-Image. Princeton, NJ: Princeton University Press.
- Roth, A.D. & Fonagy, P. (1996). What Works for Whom? A Critical Review of Psychotherapy Research. New York: Guilford Press.
- Thompson-Brenner, H., & Westen, D. (2005 a). A naturalistic study of psychotherapy for bulimia nervosa, part 1: Co morbidity and therapeutic outcome. The Journal of Nervous and Mental Disorders, 193, 573-584.
- Thompson-Brenner, H., & Westen, D. (2005 b). A naturalistic study of psychotherapy for bulimia nervosa, part 2: Therapeutic interventions in the community. The Journal of Nervous and Mental Disorders, 193, 585-595.
- Tuschen-Caffier, B., Pook, M., & Frank, M. (2001). Evaluation of manual-based cognitive-behavioural therapy for bulimia nervosa in a service setting. Behaviour Research and Therapy, 39, 299-308.
- Von Ranson, K.M., & Robinson, K.E. (2006). Who is providing what type of psychotherapy to eating disorder clients? A survey. International Journal of Eating Disorders, 39, 27-34.
- Vrabel, K.R., Rosenvinge, J.H., Hoffart, A., & Martinsen, E.W. (2008). The course of illness following inpatient treatment of adults with longstanding eating disorders: a 5 year follow-up. International Journal of Eating Disorders, 41, 224-32.
- Wilson , G.T. & Fairburn, C.G. (1998). Treatment of eating disorders. In P.E. Nathan, & J.M. Gorman, Treatments that work (pp. 501-530). New York: Oxford University Press
- Westen & Hardern-Fischer (2001) Personality profiles in eating disorders: Re-thinking the distinction between Axis I and Axis II. American Journal of Psychiatry, 2001, 158, 547-562.
- Westen, D., Novotony, C., & Thompson-Brenner, H. (2004). The empirical status of empirically supported therapies: Assumptions, methods and findings. Psychological Bulletin, 130: 631-663.
- Wilfrey, D.E. Agras, W.S., Telch, C.F., Rossiter, E.M., Schneider, J.A., Golomb Cole, A., Sifford, L. & Raeburn, S.D. (1993). Group cognitive behaviour therapy and group interpersonal psychotherapy for the non-purging bulimic individual: A controlled comparison. Journal of Consulting and Clinical Psychology, 61, 296-305.